What Contributes to Pelvic Pain?
A thorough discussion about the science of pain is beyond the scope of this article. Nevertheless, I think it’s important to highlight 2 key points about pain:
- Pain less than 3 months duration:
- This is most often caused by “tissue injury” and gradually improves over time as the tissues heal. In the case of cancer-related pelvic pain, this could be due tissue changes directly related to surgery, radiation or the cancer itself.
- Pain lasting longer than 3 months (called persistent pain):
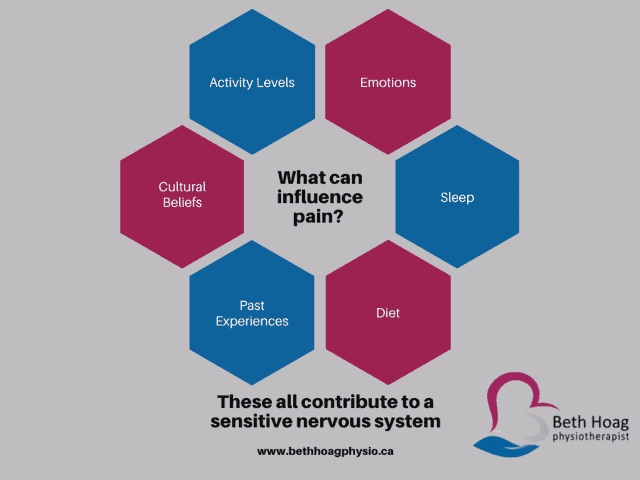
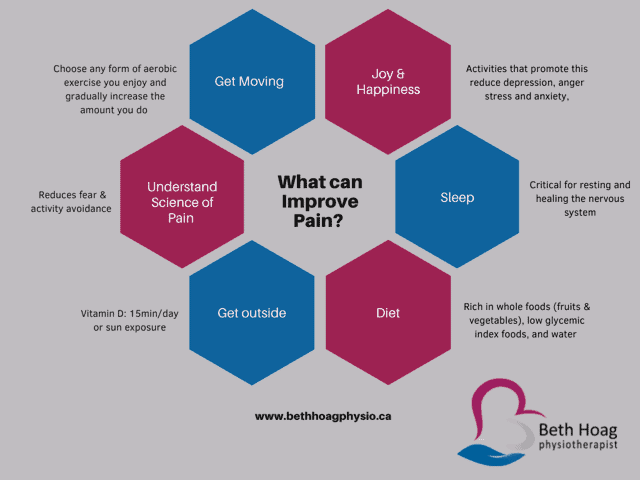
- This type of pain becomes more complex. There is an enormous amount of science showing that our nervous system (including the brain) begins to adapt and become sensitized after prolonged exposure to pain. As a result, there are many more factors that contribute to pain that lasts longer than 3 months. (See the diagram below.)
- In the case of cancer-related pelvic pain there are many other factors that can contribute to longer-lasting pain. These factors could include stress, anxiety, trauma, fear of death or cancer recurrence, poor sleep, altered diet, and lower activity levels, just to name a few.
There is also a wonderful short video
that explains pain in a simple way
Pelvic Pain and Cancer – What Causes This?
Pelvic pain during and after cancer treatment is extremely common. This is true for many women being treated for a gynecological cancer (i.e. ovarian, uterine, cervical, vaginal, vulvar) but also individuals being treated for colorectal cancer, bladder cancer and even breast cancer!
As I mentioned earlier, pain can initially be caused by surgery, radiation and even the cancer itself. It can also be a secondary effect of being put into menopause (due to surgery or hormonal therapy).
This pain can be present on a constant or intermittent (i.e. “comes and goes”) basis. It can be related to certain positions or movements and can be anywhere in the genitals and lower abdomen. Though I’m talking only about pelvic pain here, it’s important to mention that persistent low back and hip pain can be related to pelvic pain, so if you had low back and/or hip problems prior to your cancer diagnosis, this could contribute to the problem (or you could have had pre-existing pelvic floor problem that went undiagnosed.)
Common Causes of Cancer-Related Pelvic Pain
The most common causes of pelvic pain that I see in my practice are listed below. Though many of these problems are originally caused by the cancer treatments, they almost always involve other factors that are contributing to their pain (see my diagram above.)
- Myofascial restrictions in the abdomen (including scar tissue restrictions)
- Increased pelvic muscle tone
- Hip and low back restrictions
- Vulvovaginal dryness
- Vaginal narrowing (called “stenosis”)
- High levels of stress and anxiety
How to Improve your Pelvic Pain
Treating pelvic pain requires an accurate diagnosis. First, you should always tell your medical team about your pelvic pain, in case they need to run any medical tests. In addition, reaching out to a Cancer Rehabilitation Physiotherapist who is also trained in Pelvic Health will help you accurately identify the cause(s) of your pain.
There are many things you can do to improve your pelvic pain. Remember, there is no “one size fits all” for pain management, so the graphic below provides general suggestions only.
3 Things YOU can do to Improve your Pelvic Pain
- Stress really “fuels the fire” for pain. We cannot control stress but we can find ways to manage it and “keep it in check”. Deep breathing is a very simple way to calm our nervous system when we are feeling stressed.
- Try lying down in a comfortable position and breathe in through your nose, filling your belly and lower ribs with air. Exhale for twice as long as you inhale. Repeat this for 3-5mins, several times a day
- Click here for a video on deep breathing
- This is a great position to both open the pelvic floor muscles and to a supportive position for our body. Combined with deep breathing it can be incredibly calming for our nervous system.
- Click here for a video on wide-legged child’s pose
Get moving
- Do some form of exercise every day. Try to pick something you enjoy doing: walking with a friend, dancing to your favourite song or joining in a group fitness class. Even 5 minutes, 2-3x/day is better than nothing.
Pelvic Health After Cancer Matters!
Just because you’ve had cancer, does not mean that your pelvic health has to suffer. If you are experiencing pelvic pain, there is help out there.
If the above tips aren’t enough, I encourage you to reach out to a local physiotherapist (with training in cancer rehabilitation and pelvic health). If you’re having difficulty finding this person, please feel free to reach out to me directly.
Let’s start normalizing discussions about pelvic health during and after cancer!
If you found this blog helpful, please feel free to share it with someone else who could benefit from the information. Or better yet, encourage them to join my mailing list to receive my monthly newsletters and updates.
Disclaimer – These blogs are for general information purposes only. Medical information changes daily, so information contained within these blogs may become outdated over time. In addition, please be aware that the information contained in these blogs is not intended as a substitute for medical advice or treatment and you should always consult a licensed health care professional for advice specific to your treatment or condition. Any reliance you place on this information is therefore strictly at your own risk.
References
Canadian Cancer Statistics Advisory Committee. Canadian Cancer Statistics 2019. Toronto, ON: Canadian Cancer Society; 2019. Available at: cancer.ca/Canadian-Cancer-Statistics-2019-EN (accessed April 2, 2021).