What is a Neck Dissection?
In addition to removal of the tumor and possible reconstruction of the area where the tumor was removed (if the tissue removed was very large), a neck dissection is quite common. A neck dissection (also called a cervical lymph node dissection) involves the removal of lymph nodes from the neck (often on just one side.)
The lymph nodes are part of the lymphatic system, which is both a fluid and waste-removal system that also helps the body fight infections (i.e. is part of our immune system.) In the case of cancers of the head and neck, the cancer can often spread to the nearby lymph nodes of the neck, called the cervical lymph nodes. This is why a lymph node dissection is often performed.
3 Types of Neck Dissections
There are 3 main types of neck dissections, which are based on the number of lymph nodes and tissues that are removed (there are over 300 lymph nodes in the neck). The type of neck dissection has a direct impact on the level of shoulder function and recovery (3).
- Radical Neck Dissection
This involves the removal of the majority of lymph nodes on one side of the neck, in addition to the internal jugular vein, sternocleidomastoid muscle and spinal accessory nerve. Due to the removal of the spinal accessory nerve (which supplies the trapezius muscle), the long-term impact on the shoulder is significant. The shoulder and shoulder blade will be visibly drooped and it will not be possible to actively raise the shoulder above shoulder-height. Discomfort to the neck and collarbone can also develop over time. Due to the significant impact on overall function, this type of neck dissection is done far less frequently than in the past.
- Modified Radical Neck Dissection
This operation involves the removal of a large number of lymph nodes on one side of the neck, in addition to one or more of the internal jugular vein, sternocleidomastoid muscle and spinal accessory nerve. The impact on the shoulder function is completely dependent on the number of “additional structures” removed. When compared to a radical dissection, it is more common for the impact on the shoulder and neck to be less severe and it is can sometimes be temporary (if rehab support & exercises are performed)
- Selective Neck Dissection
This operation involves the least amount of disruption to the neck. Fewer lymph nodes are removed and the surrounding muscles, nerves and blood vessels remain in place. Though shoulder and neck function will be initially impacted, it is typically temporary, when the proper exercises and rehab support are performed.
Anatomy: What is the Spinal Accessory Nerve?
The spinal accessory nerve (also known as cranial nerve XI) is the nerve that communicates with the trapezius and sternocleidomastoid muscles. The trapezius muscle is essential for proper functioning of the shoulder girdle (i.e. shoulder blade, collarbone, and shoulder joint). The sternocleidomastoid muscle is important for movement of the neck.
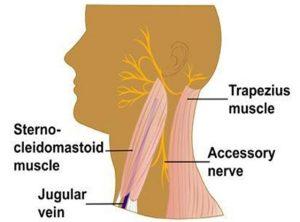
(Photo credit: the American Head & Neck Society: https://www.ahns.info/neck-dissection/)
Anatomy: What is the Trapezius Muscle?
The trapezius muscle runs from the base of your skull and attaches directly to the shoulder blade (i.e. scapula), collarbone and mid-back (i.e. thoracic spine). The job of the trapezius is to control the movement of the shoulder blade.

Shoulder blade control is essential for healthy shoulder movement; think of the shoulder blade a bit like the foundation of your house (the shoulder). If the foundation of your home isn’t solid then the rest of the walls begin to lean, doors won’t open/shut properly and you may start to see cracks in your walls. If the shoulder blade doesn’t sit in a healthy position and doesn’t move properly, then the shoulder itself cannot move properly. This will show up as a loss of shoulder mobility, pain and possible injuries later on. (Poor shoulder blade control also has a pretty significant impact on other areas of the body such as your neck, collar bone and upper ribs, but this is too complicated to discuss in this blog!)
The Degree of Nerve Disruption Predicts Shoulder Function
The accessory nerve can be impacted in several ways during a neck dissection.
Permanent injury can occur when the nerve has been completely severed (i.e. cut) or if the nerve has been significantly stretched beyond its capacity (i.e. nerves have some elasticity, but can only stretch so far before being injured.)
Temporary injury can occur when the nerve has been severed but surgically reattached and/or overstretched. Note, however, that there is a significant amount of variability in how much the nerve will recover over time.
A nerve can also be injured with compression, but this is extremely uncommon with a neck dissection surgery. Traction (or stretching) injuries are much more common and are related to when the nerve has been “moved out of the way” for your surgeon to access the tissues that need to be surgically removed.
3 Ways to Maximize Your Shoulder Outcome After a Neck Dissection
1. Know what happened to your accessory nerve
As I mentioned previously, there is an enormous amount of variability with respect to how much the accessory nerve will recover over time, if at all. The most important variable to consider, is what happened to your accessory nerve during your surgery.
During your surgical follow up, ask your surgeon what happened to your accessory nerve during surgery: was it cut, cut and sewn back together, stretched/retracted (most common), or untouched (unlikely)? This is critical in being able to predict how much you can expect the nerve (and thus your shoulder function) to recover.
2. Start with shoulder shrugs
Assuming your nerve was not removed or cut, shoulder shrugs can be a great place to start your recovery. Use the trapezius muscle to raise the shoulders up and down. Even if you cannot physically do the exercise, getting yourself into the position and visualizing yourself doing it can help begin to restore the connection between the nerve and the muscle. Be consistent with this exercise and be patient; it can take months for the nerve and the muscle to restore their “communication.” Want to learn how to do this exercise? I have created a video of this exercise to help you out.

3. See an experienced cancer rehab physiotherapist
Ultimately, the shoulder girdle is complex. Seeing a cancer rehab physiotherapist can be a really useful way to get help progressing beyond this simple shoulder shrug exercise into more complex and functional movement patterns.
(April is National Oral, Head & Neck Cancer Awareness Month. Please share this blog with someone you know who is facing or recovering from a neck dissection surgery. Let’s help them get the support they need to recover.)
References
1) Canadian Cancer Society. 2022. Head and Neck Cancer Statistics. https://cancer.ca/en/cancer-information/cancer-types/oral/statistics
2) Lima, L. P., Amar, A., & Lehn, C. N. (2011). Spinal accessory nerve neuropathy following neck dissection. Brazilian journal of otorhinolaryngology, 77(2), 259–262. https://doi.org/10.1590/s1808-86942011000200017
3) Larsen MH, Lorenzen MM, Bakholdt V, Sørensen JA. The prevalence of nerve injuries following neck dissections – a systematic review and meta-analysis. Dan Med J. 2020 Aug 1;67(8):A08190464. PMID: 32741441.
Disclaimer – These blogs are for general information purposes only. Medical information changes daily, so information contained within these blogs may become outdated over time. In addition, please be aware that the information contained in these blogs is not intended as a substitute for medical advice or treatment and you should always consult a licensed health care professional for advice specific to your treatment or condition. Any reliance you place on this information is therefore strictly at your own risk.