So, if your cancer treatments are leaving you struggling with constipation, please know that you are not alone. (In fact… you’re pretty much normal!)
But who likes to talk about poop? I do!
As a physiotherapist working in cancer rehab and pelvic health, I talk about poop… A LOT! In this blog, we’re going to discuss how you know if you have constipation, what you can do to help manage it, and when to reach out for more help.
What is Constipation?
Before we talk about constipation, it’s helpful to know what is considered “optimal” bowel health. Normal bowel movement frequency ranges widely between 2-3x/day to 3x/week. The consistency of your stool should be relatively soft and easy to pass. A common way I help clients identify their stool consistency is to refer to the Bristol Stool Chart; healthy stool should range between a type 3 or 4.
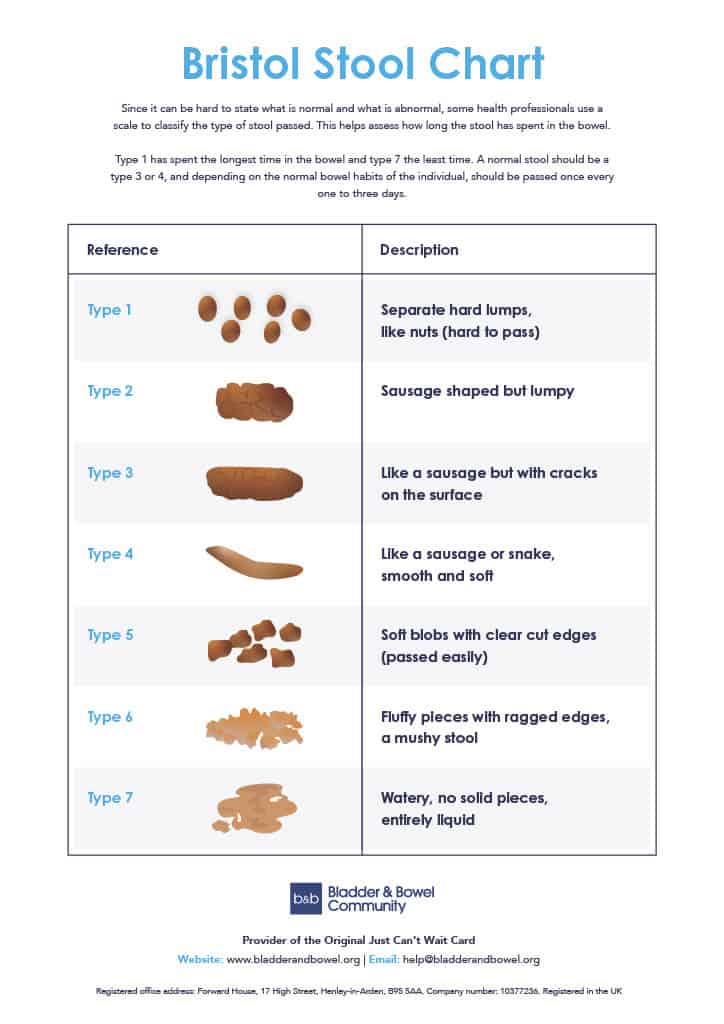
In contrast, constipation is when you have bowel movements less often than your normal and the consistency is harder and more difficult to pass (Bristol stool chart types 1 and 2).
How does cancer treatment cause constipation?
Though it’s important to speak with your medical team to understand your specific situation, there are common reasons why you may experience constipation during cancer treatment:
- Pain medications (especially narcotics) can slow your bowels down
- Certain chemotherapy and anti-nausea medications
- Eating and drinking less
- Cancers of the belly, pelvis and/or bowel may put pressure on your bowels
- Increased pelvic floor muscle tone due to pain and/or stress
Constipation Signs to Watch For
Constipation can show up in a variety of ways; it’s not always as simple as “just not pooping.” The following is a list of possible signs that you may be constipated:
- Less frequent bowel movements than your usual
- Bowel movements that are hard, small and pellet-like
- Painful bowel movements
- Feeling the need to strain or bear-down to pass stool
- Gas and/or burping
- Bloating and/or feeling full in the belly
- Stomach aching/cramping
- Nausea/vomiting
10 Things YOU Can do to Promote Healthy Bowels during cancer treatment
We cannot fully control and undo the impact that certain cancer treatments have on your bowels, but the evidence shows that diet and lifestyle modifications can play an important part in preventing and/or managing constipation during cancer treatment (2). It is also my experience, working in pelvic health, that toileting positions and habits can also be very helpful in promoting healthy bowel movements.
1. Drink more fluids (3)
Many of my cancer rehab clients struggle to stay well-hydrated during cancer treatment (and beyond… let’s be honest!) Unless your medical team has advised you otherwise, aim to drink 6-8 glasses of fluid every day. Warming your drinks can also be helpful for your bowels. Adding flavour to your drink (like a splash of lemon) can help altered tastebuds caused by chemotherapy.
2. Move Every Day (3)
Here is yet another reason why movement is medicine! I know that exercise during cancer treatment can be challenging but getting movement each and every day is extremely helpful for your bowels. Aim for 20-30minutes a day of something physical (like walking… or my personal favourite… kitchen dance parties). You can also break it up into smaller periods (e.g. 3 x 10mins) if you’re having a difficult day. If you just can’t get out of bed, try moving your joints: do 10 repetitions per joint, moving from head to toe (e.g. neck turns, shoulder circles, elbow bends, etc.). Something is definitely better than nothing!
3. Increase Fiber in Your Diet (maybe)
Gradually adding more fiber to your diet can be a helpful way to soften your stool and make it easier to pass (note: doing it too quickly can cause gas and stomach upset.) Basic foods like brown rice, whole grains, fruits, vegetables, seeds and nuts are all great sources of fiber. (Speak with a dietician to obtain more detailed information about healthy sources of fiber.) However, if you are taking opioid pain medication (like morphine), speak with your healthcare team to decide if eating more fiber is the right solution for you.
4. Do NOT Delay the Urge to Void (i.e. poop)
Your bowel is not designed as a “long-term storage tank”; the longer that stool stays in your body, the more water can be drawn out of your stool (creating harder poop!) As such, when you feel the urge to have a bowel movement, do not ignore your body’s wisdom. Calmly find a toilet and get down to business!
5. Develop a Bowel Routine
Your bowels LOVE habit and routine…. They “sleep” at night and are “active” during the day. Though everyone’s bowels behave a little differently, the best time to have a bowel movement is generally about 30minutes after your first meal of the day. With this in mind, carve out enough time in your morning to have 5-10 minutes of rush-free time in the bathroom. If you rarely feel “the urge” to void, going through the motions of this morning routine (i.e. actually sit on the toilet for 5mins while trying some of the tricks below) can help your bowels associate this time with voiding.
6. Put Your Feet up on a Stool
Your bowels work best in a “squat-like” position. This position relaxes the muscles at the around your anus and “straightens the angle” in your lower bowel (called the anorectal angle). As a result, this position makes it easier to have a bowel movement. Placing your feet flat on an 8-12 inch stool can really help. The exact stool height should allow your knees to be higher than your hips, while maintaining contact with your sit bones on the toilet seat (i.e. you don’t have your “tail tucked between your legs”). Keep your feet and knees separated comfortably and rest your elbows on your knees.
7. Deep Breathing
Your diaphragm (i.e. your “breathing muscle”) is linked to your pelvic floor muscles. As you breathe in, your pelvic floor muscles relax, making bowel movements easier. Deep breathing also “pumps and massages” the intestines which can further help. So, as you sit with your feet on a stool, focus on diaphragmatic breathing to get your bowels moving.
8. Twist Instead of Straining
While seated on the toilet, try slowly turning your upper body to the right and deep breathing while you hold this position. Repeat this while turning to the left. This can help gently move the stool into the rectum.
9. Tilt Your Pelvis
In addition to deep breathing and twisting, tilting your pelvis forward and backwards can also help move stool into the rectum. Imagine you have a “bunny tail” at the back of your pelvis, then move between “tucking your tail between your legs” to “sticking your tail out back.”
10. Massage your Belly (ILU)
Massaging your belly can help increase the movement of the digested food in your intestines (called chyme). Done 1-2x/day, this technique can help improve your bowel health. The nickname for this technique is “I Love U” to help remember the steps. Here are the steps for this technique (Repeat each step 10-15x):
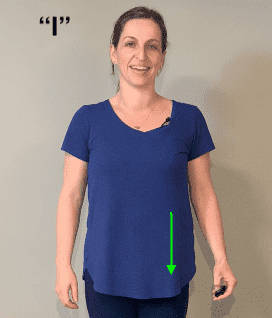
- “I”
- Begin on the left side of your belly, using firm pressure to sweep from the top of your belly (by the ribs) to your left lower belly.
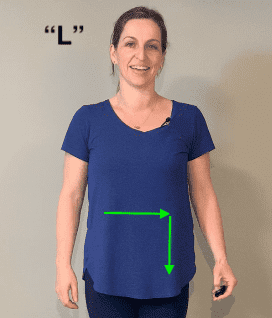
- “L”
- Next, in the shape of an “L”, use a firm and continuous sweep starting in the R upper quadrant of your belly (near your ribs), over the L upper belly, then down to your L lower belly. (When you look down at your belly, you are drawing an “L”)
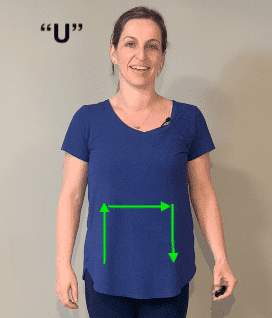
- “U”
- Finally, in the shape of a “U”, use a firm and continuous sweep, starting in the R lower quadrant of your belly, up to the right upper quadrant, then over to left upper and then left lower quadrants. (When you look down at your belly, you are drawing a “U”)
When to Contact your Medical Team?
Finally, any changes your health should always be reported to your medical team. In the case of constipation, your medical team should be promptly contacted if you have any of the following:
- You have not had a bowel movement in 2-3 days
- There is blood in your stool
- Your stool is black
- You have belly cramps for more than 2 days
Interested in learning more about how cancer can impact your pelvic health? Check out some of my other blogs:
- Pelvic Pain after Cancer: The Silent Problem
- Breast Cancer and Pelvic Health
- Pelvic Health after Gynecological Cancer
- Moisturizers and Lubricants to Improve Vaginal Dryness
Until next time, be well.
Beth
Disclaimer – These blogs are for general information purposes only. Medical information changes daily, so information contained within these blogs may become outdated over time. In addition, please be aware that the information contained in these blogs is not intended as a substitute for medical advice or treatment and you should always consult a licensed health care professional for advice specific to your treatment or condition. Any reliance you place on this information is therefore strictly at your own risk.
References
- McMillan, S.C. et al. (2013). Trajectory of medication-induced constipation in patients with cancer. Oncology Nursing Forum, 40(3), E92-E100. https://doi.org/10.1188/13.ONF.E92-E100
- Rogers, B., Ginex, P. K., Anbari, A., Hanson, B. J., LeFebvre, K. B., Lopez, R., Thorpe, D. M., Wolles, B., Moriarty, K. A., Maloney, C., Vrabel, M., & Morgan, R. L. (2020). ONS Guidelines™ for Opioid-Induced and Non-Opioid-Related Cancer Constipation. Oncology nursing forum, 47(6), 671–691.
- Cancer Care Ontario. (February 2016 ). Constipation During Cancer Treatment. https://www.cancercareontario.ca/sites/ccocancercare/files/assets/CCOConstipationCancerTreatment.pdf?download=1