Traditionally, the goal of this month is to raise awareness about the signs and symptoms of gynecological cancer so that women are more likely to detect their cancer earlier. While this is extremely important (as many of the symptoms can be vague and subtle), I also want to raise awareness about the importance of maximizing quality of life during and after treatment for women diagnosed with a gynecological cancer
The Numbers Don’t Lie
48% of women with a newly diagnosed cancer in Canada will have a cancer that may negatively impact their pelvic health. For men, this number is 45%. (Canadian Cancer Society)
Problems such as bladder and bowel incontinence (leaking), constipation, pelvic pain, and changes in sexual function are very common for these people and can have a significant impact on quality of life.
Unfortunately, our attention in cancer care remains focused on survival rates alone; quantity of life is the focus. This has brought about impressive improvements in survival rates, but as treatments continue to improve, more people than ever before are now living with the lasting side effects of their cancer treatment. Sadly these very same people are not receiving enough support in managing their treatment side effects; quality of life is being sacrificed.
As a result, many people affected by cancer are left to either suffer in silence or take it upon themselves to find the help they need. This is no different for those who experience pelvic health side effects after treatment for gynecological cancer.
Pelvic Health: The pattern I couldn’t ignore
During the first 9 years of my cancer rehabilitation practice, I would often refer my clients out to pelvic health physiotherapists to address their pelvic health needs. Not infrequently, however, I would receive feedback from my clients that they felt “out of place” in these clinics, as many were focused on pre- and post-natal care for new mothers. Although they really liked their pelvic health physiotherapist, some were concerned that these physios had little experience with “cancer-related issues.”
Combining Cancer Rehab and Pelvic Health
After experiencing this for several years, I decided to take my pelvic health training in 2017 with the specific intent to meet the unique needs of individuals affected by cancer. Since this time, I screen each and every one of my clients for pelvic health problems, even if they do not state this as their reason for consulting me. This is one aspect of my belief in treating the whole person.
“No one has ever asked me about this before.”
“I had no idea this could happen to me.”
“I thought I just had to live with it.”
These are the common responses I get when we discuss the pelvic health screening questions I ask. Not only is it astonishing that so few women are ever asked these questions, but more shocking is how many women answer “yes” to at least one question; they have been suffering in silence (sometimes for years) thinking they “just had to live with it.”

You Are Not Alone
Through a growing body of scientific research, we know that the number of women who experience pelvic health problems after gynecological cancer treatments is quite high. 50.9% of these women report urinary difficulties, 42% report bowel difficulties, and 48.5% report sexual dysfunction (Westin et al 2016). Other studies report even higher rates of these problems. Regardless of the specific number, it is crystal clear that many women are experiencing pelvic floor problems after gynecological cancers.
If you are one of these women, you are not alone.
Why aren’t Women Getting Help?
“It could be worse”
“I am grateful to be alive. I feel guilty complaining about this.”
These thoughts are very common in women affected by cancer. As a result, we know that many women are not reporting their pelvic floor concerns (and this is why I screen all of my clients for pelvic health problems). In other words, the number of women reported to be experiencing pelvic floor dysfunction after gynecological cancer treatment (as discussed above), is likely an underestimation.
I personally hear many women make the above comments in my practice. Though I am humbled by their gratitude and outlook on life, over my years of work in cancer rehabilitation, I have come to appreciate that these women deserve so much more than “survival” alone. As a result, I now regularly challenge their thinking and suggest that they have the right to live WELL during and after cancer.
Just because you’ve had cancer does not mean you have to suffer.
Gynecological Cancers and Pelvic Health
Treatments for gynecological cancers may include surgery, chemotherapy, radiation therapy and hormone therapy. There are a wide range of treatment side effects that can be helped by physiotherapy, but the level and depth of assistance you receive will depend on the training and knowledge of your physiotherapist. See below for a graphic I created to help explain this:
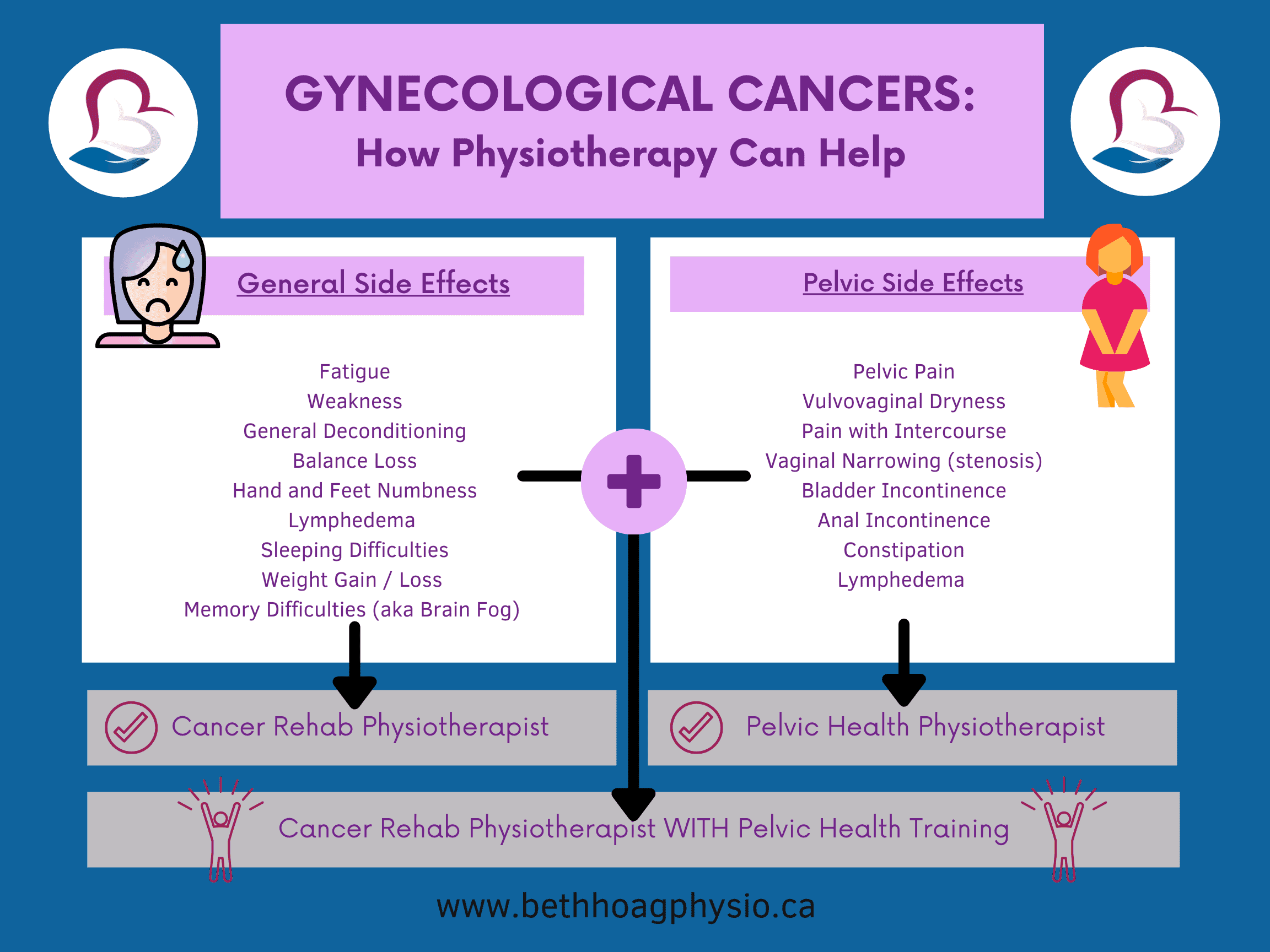
Finding Help
Finding a pelvic health physiotherapist who is also knowledgeable in cancer rehabilitation may be difficult for many women to find. Both fields of physiotherapy are still emerging specialties, and the combination of them both is even more rare. Nevertheless, you can still find the help you need.
It’s ok to ask questions to find the right therapist to help you.
If you find a pelvic health physiotherapist in your area, ask them if they have any experience working with women who’ve had your type of cancer (or any type of gynecological cancer). If you find a cancer rehabilitation physiotherapist in your area, ask them if they have training in pelvic physiotherapy. If either practitioner answers no, ask them if they know someone who does. If none of this is possible, many physiotherapists offer virtual appointments so you may be able to work with someone far away. (Note: I offer one-on-one Cancer Rehab services to anyone in the province of Ontario, Canada).
Finally, if you’re experiencing ANY of the symptoms listed in the graphic above, please know that there IS help out there.
If you have any questions or would like help managing your symptoms, please don’t hesitate to reach out to me directly.
References
- Canadian Cancer Statistics Advisory Committee. Canadian Cancer Statistics 2019. Toronto, ON: Canadian Cancer Society; 2019. Available at: cancer.ca/Canadian-Cancer-Statistics-2019-EN . Accessed April 17, 2021.
- Westin SN, Sun CC, Tung CS, Lacour RA, Meyer LA, Urbauer DL, Frumovitz MM, Lu KH, Bodurka DC. Survivors of Gynecologic Malignancies: Impact of Treatment on Health and Well-being. J Cancer Surviv. 2016 Apr;10(2):261-70
Disclaimer – These blogs are for general information purposes only. Medical information changes daily, so information contained within these blogs may become outdated over time. In addition, please be aware that the information contained in these blogs is not intended as a substitute for medical advice or treatment and you should always consult a licensed health care professional for advice specific to your treatment or condition. Any reliance you place on this information is therefore strictly at your own risk.