When I assess how my cancer rehab clients are breathing and we begin to correct things, many are surprised to experience how much better it feels in their bodies when they actually breathe properly!
Read on to learn how you can use your breath to help you feel better during and after cancer treatment.
The Diaphragm: Where It All Begins
The primary muscle responsible for breathing is called the diaphragm. It sits like a dome up in your ribcage and it attaches to your lower ribs, upper lumbar spine (i.e. your low back area), as well as other muscles and fascia.
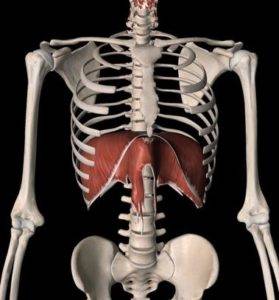
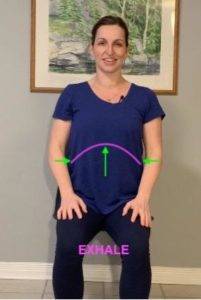
When you take a breath in (inhale), the diaphragm muscle contracts. As it does this, it widens by spreading your ribs outward and lowering down toward your belly. As you breathe out (exhale), your diaphragm muscle relaxes, rises back up under the ribcage and your ribs come closer together.

(Fun fact: When functioning optimally, your pelvic floor muscles actually mirror the movement of your diaphragm!)
EVERYTHING Is Connected
“The hip bone’s connect to the…..” Remember this song? Well there’s a lot of wisdom to it!
Even though the diaphragm is our primary breathing muscle, there are many other muscles and fascia that are involved in allowing you to breathe optimally. In addition, your ribs have to move properly to allow other part of your body to move freely. In other words… it’s all connected and it’s all related!
I won’t get into the specifics of all of these connections in today’s blog, but for now simply consider your diaphragm as part of “the foundation of your home.” You need a well-functioning foundation to support your walls (i.e. your arms, legs, head and neck.)
5 Reasons Why Diaphragmatic Breathing is Helpful if You’ve Had Cancer
1 – Relaxation
Many studies have shown that focusing on breathwork is an effective way to help lower and manage stress. Though it does take some practice and commitment, as little as 3 minutes a day of slow, deep breathing can make a difference. You can also use this simple technique to calm your nerves as you sit in the waiting room for your oncologist or as you’re going through your cancer treatment.
2 – Pain Management
There is also a lot of pain science research showing that deep breathing (as a form of meditation or mindfulness practice) can be an effective way to manage pain. When done with awareness, deep breathing can help to calm your nervous system which can, in turn, significantly ease the intensity of pain and discomfort you may be experiencing during cancer treatment.
3- Rib movement
As I mentioned earlier in this blog, everything is connected! Rib movement occurs in conjunction with most of the things we do every day: walking, going up and down the stairs, getting in the car, picking up your laundry basket, reaching into your kitchen cupboard for a glass, etc. As a result, using deep breathing is a great way to maximize some of your rehab exercises after cancer surgery and radiation.
4 – Promoting lymphatic flow
The largest lymphatic vessel of the body, called the thoracic duct, goes through the diaphragm. As a result, every deep breath that you take acts like a bit of a “sump pump” to help move lymphatic fluid through your body. If you have cancer-related lymphedema, this is one important technique to help promote lymphatic drainage and flow.
5 – Optimizing pelvic health
If you caught my “fun fact” earlier in this blog, you already know that the diaphragm and pelvic floor muscles work together. As such, promoting proper diaphragmatic breathing is a key building block to optimizing pelvic health (e.g. to reduce bladder leaks, pelvic pain, symptomatic prolapse and promote bowel health).
How to Use Your Diaphragm to Breathe?
Lying down on your back with your knees bent, place your hands on either side of your lower ribs. Begin by taking slow, relaxed breaths in and out. Take a few breaths and notice where in the body you feel the breath (e.g. Neck? Upper chest? In your hands? In your belly?) and how much your hands are being moved by the breath.
Next, visualize an upside down umbrella deep inside your ribcage; the handle is by your chin and the tip is above your belly button. As you breathe in, visualize the movement beginning in your lower ribs where your hands are placed. Feel this area expand like an umbrella being opened up 360 degrees into your hands (front & back, left & right). As you exhale gently (not forced) visualize the umbrella becoming smaller and feel your hands come closer together again.
If you’d like more guidance on this technique, head to my YouTube Page for a video to guide you through deep breathing exercise.
Incorporating Diaphragmatic Breathing Into Other Cancer Rehab Exercises
In my online Breast Cancer Surgery Recovery Program, we integrate diaphragmatic breathing into all of the rehab exercises. Each exercise is explained through a detailed video that guides you through the movement and includes specific cues on how to coordinate your breath with the movement. If you’d like to learn more about this online program, click here.
Until next time, be well.
Beth
Disclaimer – These blogs are for general information purposes only. Medical information changes daily, so information contained within these blogs may become outdated over time. In addition, please be aware that the information contained in these blogs is not intended as a substitute for medical advice or treatment and you should always consult a licensed health care professional for advice specific to your treatment or condition. Any reliance you place on this information is therefore strictly at your own risk.