What is Considered a ‘Normal’ Bowel Routine?
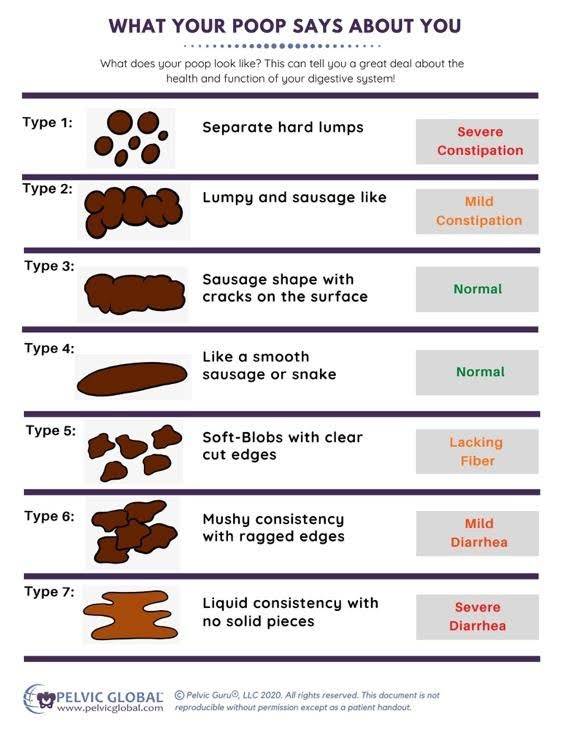
First, we need to discuss what constitutes a normal bowel routine. Typically, normal bowel movement frequency ranges anywhere from 3x/day to 3x/week. I know this seems like a really large range, but we’re all a little different when it comes to bowel movements! In addition, stool consistency should be a 3-4 on the Bristol Stool Chart (see the diagram below to understand what that is!)
What is Constipation During Chemotherapy and Cancer?
Based on the above description of normal bowel movements, constipation occurs when we have fewer than 3 bowel movements a week. You might also notice that your bowel movements are firm small pellets or even just hard to pass. This would be considered a type 1 or 2 stool on the Bristol Stool Chart.
Why Does Being Constipated Matter?
Though constipation may not seem like a big deal, constipation during chemotherapy can be physically and emotionally distressing and sometimes even painful:
- The state of being constipated can cause general discomfort
- Having a bowel movement when constipated can be really difficult and downright painful (sometimes even contributing to hemorrhoids and fissures)
- Constipation can contribute to low back pain and negatively impact bladder health (you read that right… bowel and bladder health are related!)
- Being constipated can be really frustrating and emotionally distressing
How Digestion Leads to Bowel Movements
Before we go any further, I think it’s important very briefly to talk about how digestion works.
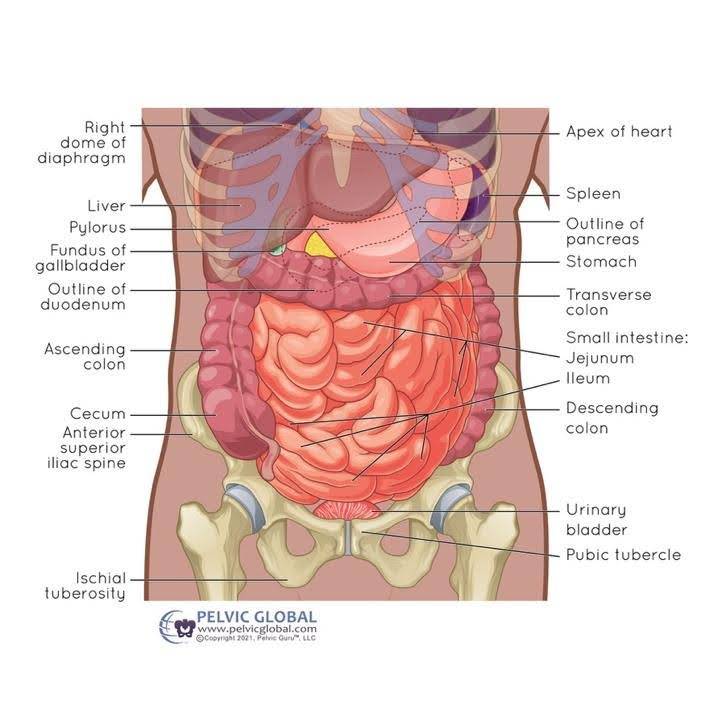
Think about your digestive system like two ends of a tube with an entry point and an exit point. When we eat food (entry point), digestion begins with chewing and saliva. This food then passes to our stomach via the esophagus, a tube which connects our mouth to our stomach.
Once it enters the stomach, different digestive juices and enzymes help to further digest that food. It then enters our small intestine, which is a long, winding length of tube that is in our stomach. As our “digested food” passes through the small intestine, our body absorbs essential nutrients in order to support our energy needs.
Once it leaves the small intestine, it enters our large intestine (aka the colon), which is shaped a bit like an upside-down U in our stomach. Although there’s still absorption that happens in the large intestine, the primary role of this part of our digestive system is to transport and temporarily store stool for short periods of time, before it leaves our body. Stool then passes into the rectum before leaving our body through the anus.
Why Does Constipation During Chemotherapy and Cancer Treatment Happen?
The two most common reasons why constipation during chemotherapy happens are as follows:
1. Slow movement of stool through the large intestine
This is the most common cause of constipation during cancer treatment. A large part of this slowed transit time is related to a variety of medications used during chemotherapy and other cancer treatments. The consequence of stool staying longer in the large intestine is that there is more time for more water to be reabsorbed back into the body. As a result, stool becomes drier over time, which then makes it more difficult to pass.
2. Increased tone around the muscles of the pelvic floor
The pelvic floor muscles, which sit at the bottom of our bony pelvis, have multiple functions including contributing to bowel health. When these muscles have more tone than usual, they make it difficult to have a bowel movement.
What Can You Do To Manage Constipation During Chemotherapy and Cancer Treatment?
The good news is that there are multiple ways to help soften your stool and get things moving! Here are my top tips:
1. Get Moving:
Our bowels need regular movement. I know this can be difficult when you’re going through chemotherapy, but a little bit goes a long way. Aim to get some regular physical activity for 20-30 minutes a day. If you’re feeling really tired during chemotherapy, pacing yourself is important; spread those 20-30 minutes over the course of your day. Walking is a simple place to start.
2. Regular Mindful Moments:
Our bowels do not respond well to stress. When our nervous system is in a heightened “fight or flight” state, our bowels slow down, which can contribute to constipation. Though we can’t avoid the stressful reality of cancer, we can work to “dip” your nervous system into a different experience multiple times a day, which will also help your bowels. If you’re interested in learning more about different strategies that you can use, I have a few great videos of different mindfulness practices on my YouTube channel
3. Start a Bowel-Friendly Morning Routine:
Our bowels also love routine! Starting your day with a quiet and calm routine (remember point #2 above about dipping into moments of relaxation?) can get your bowels moving and set you up for success. It takes practice and repetition for your bowels to “get the hint.” Here are a few tips:
- Coffee lovers unite: Start your day with a warm drink. If you like coffee… good news! Coffee is a really great bowel stimulant.
- Massage your belly: Adding a simple belly massage (called the ILU massage) can increase its motility and get things moving at a faster rate.
4. Deep Breathing:
This super simple act is a powerful way to “milk your gut.” When we take a deep breath in, the diaphragm lowers into the belly and thus all of your belly contents move downward as well. The reverse happens when we exhale. This repeated up-and-down motion of the gut does wonders to get your intestines moving things along! Check out this video for a really cool image of what happens to our gut when we deep breathe.
5. Body Twists:
Body twists are also a brilliant way to get our gut moving. Many yoga poses offer a variety of gentle twist poses. Add deep breathing to these stretches and your intestines will thank you. Here’s a link to one such twist pose. (Note: if you have osteoporosis or cancer lesions in your spine, please skip these twists.)
6. Stay Hydrated:
Drinking ample fluids that are non-caffeinated and non-alcoholic, helps hydrate our poop.

7. Fibre-Rich Foods:
Fibre-rich foods like green leafy vegetables and complex carbohydrates are a really helpful way to increase and bulk up your stool. If you want a little bit more advice about this, head here. One thing to note about fibre intake is that it can be helpful to speak to a local dietician about ways to increase fibre in your food to make sure that it’s appropriate for your situation, that you’re getting the right types of fibre, and that you’re bringing it in gradually so you’re not overloading your system all at once.
8. Medications to Help:
If all of the above isn’t working, I encourage you to speak to your medical team. At the end of the day, you might benefit from the use of a stool softener or laxative. However, it is critical that you have this conversation with your medical team before taking any of these, as there are sometimes reasons why one option over another is appropriate in your individual case.
Final Tip About Constipation: Don’t Ignore the Urge!
Finally, when you feel the urge to have a bowel movement, I want you to respond to that urge appropriately; walk calmly to the toilet and go have a poop!
Seriously… in this fast-paced world, people frequently delay a bowel movement because “it’s not a good time” (e.g. they’re busy doing something, they hate public bathrooms, etc…. sound familiar?!) But remember that the longer that stool stays in your colon, the more dehydrated it becomes and the harder it is to pass.
So listen to your body’s wisdom and just get to the toilet!
(Image Credits: All images labelled with “Pelvic Global” have been used with permission and tremendous appreciation.)
Disclaimer – These blogs are for general information purposes only. Medical information changes daily, so information contained within these blogs may become outdated over time. In addition, please be aware that the information contained in these blogs is not intended as a substitute for medical advice or treatment and you should always consult a licensed health care professional for advice specific to your treatment or condition. Any reliance you place on this information is therefore strictly at your own risk.