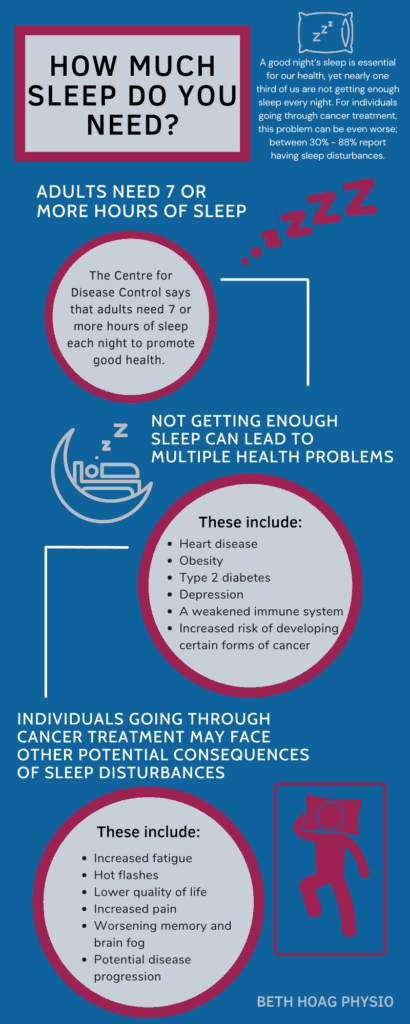
How Much Sleep do you Need?
The Centre for Disease Control says that adults need 7 or more hours of sleep each night to promote good health (1). Not getting enough sleep, can lead to multiple health problems including (1, 2):
- Heart disease
- Obesity
- Type 2 diabetes
- Depression
- A weakened immune system
- Increased risk of developing certain forms of cancer
“Adults need 7 or more hours of sleep each night.”
In addition to the above health problems, individuals going through cancer treatment may face other potential consequences of sleep disturbances (2, 4):
- Increased fatigue
- Hot flashes
- Lower quality of life
- Increased pain
- Worsening memory and brain fog
- Potential disease progression
How Cancer Treatment Impacts Sleep
Sleep can be influenced by so many factors. During cancer treatment, a combination of physical and psychological factors are likely to impact how well you sleep during cancer, and for how long. These factors can be directly caused by the cancer treatment or can be a secondary consequence of the treatment.
Direct impacts of cancer treatment on sleep:
- Steroids
- Hormone therapy
- Antidepressants
Indirect impacts of cancer treatment on sleep:
- Needing to urinate at night
- Hot flashes
- Pain
- Diarrhea
- Nausea
- Changes to sleep routine (e.g. in hospital)
- Anxiety
- Stress
- Depression
How to get a Better Night’s Sleep During Cancer Treatment and Beyond
Ultimately, we want to support your immune system during and after cancer treatment. Getting a better night’s sleep is one important way to help accomplish this.
For a better night’s rest, try these tips:
- Sleep Routine
- Go to bed and wake up at the same time every day
- Try a “wind down” activity prior to bedtime (e.g. taking a bath, reading a book, dimming the lights)
- Set the Bedroom Scene
- Keep your bedroom cool and dark
- Keep screens OUT of the bedroom (i.e. cell phones, tablets, TVs)
- Use your bedroom for sleep and sex only (so your brain associates the bedroom with ONLY these things)
- Consider using a white-noise machine or wearing ear plugs if you’re a light sleeper.
- Food and Drink
- Avoid large meals and heavy snacks close to bedtime
- Avoid alcohol late in the evening (Alcohol may help you fall asleep but it disrupts your QUALITY of sleep.)
- Avoid caffeine up to 8 hours before bedtime (Caffeine can impact our bodies for up to 10 hours!)
- Limit your fluid intake 2 hours before bedtime (so you’re less likely to need to get up to urinate at night)
- Limit Napping
- Whenever possible, limit the length of daytime naps
- Try to avoid napping after 3pm.
- Exercise Every Day
- Make daily exercise a priority and consider doing this in the morning when energy levels tend to be higher. (Note: intense exercise close to bedtime can actually disrupt your sleep, so the timing matters!)
- Regular physical activity has been shown to improve sleep quality and quantity in cancer patients (5,6).rest
What to do if you Can’t Sleep*?
- . Write it down
- If your mind is racing, keep a notebook by your bed. Writing your thoughts down can declutter your mind and help you to gear down for sleep.
- Mindfulness Practice
- Using a simple relaxation technique can both distract your mind and help calm your nervous system in preparation for sleep.
- Try taking 10 deep breaths or doing a body scan.
- If you can’t sleep after 20 minutes
- Leave the bedroom and do something relaxing in dim light until you feel sleepy again. We want your nervous system to associate the bedroom with sleep and sex only, so if you’re spending hours staring at the ceiling, you can actually be training your brain to associate the bedroom with NOT sleeping!
(*Note: It is also important to speak with your medical team about your sleep during cancer concerns, as there may be underlying medical reasons causing this that need to be investigated and treated.)
Want to Learn More About Sleep?
If you haven’t already read this book, “Why We Sleep” by Matthew Walker is absolutely fascinating! Dr. Walker is a professor of neuroscience and psychology at UC Berkeley, and explains in plain language the science behind the importance of sleep and dreaming. Well worth a read! (Note: I do not make any commissions of recommending this book… I just think that it’s worth sharing!)
Until next time, be well.
Resources:
(1) Center for Disease Control. (2020, April 15). Sleep and Sleep Disorders. Retrieved February 26, 2022, from https://www.cdc.gov/sleep/index.html
(2) Tejada, M., Viele, C., Kober, K. M., Cooper, B. A., Paul, S. M., Dunn, L. B., Hammer, M. J., Wright, F., Conley, Y. P., Levine, J. D., & Miaskowski, C. (2019). Identification of subgroups of chemotherapy patients with distinct sleep disturbance profiles and associated co-occurring symptoms. Sleep, 42(10), zsz151. https://doi.org/10.1093/sleep/zsz151
(3) Walker, M. (2017). Why We Sleep. Scribner Books.
(4) Canadian Cancer Society. (n.d.). Sleep Problems. Retrieved February 25, 2022, from https://cancer.ca/en/treatments/side-effects/sleep-problems
(5) Rogers, L. Q., Courneya, K. S., Oster, R. A., Anton, P. M., Robbs, R. S., Forero, A., & McAuley, E. (2017). Physical Activity and Sleep Quality in Breast Cancer Survivors: A Randomized Trial. Medicine and science in sports and exercise, 49(10), 2009–2015. https://doi.org/10.1249/MSS.000000000000132
(6) Medysky, M. E., Temesi, J., Culos-Reed, S. N., & Millet, G. Y. (2017). Exercise, sleep and cancer-related fatigue: Are they related?. Neurophysiologie clinique = Clinical neurophysiology, 47(2), 111–122. https://doi.org/10.1016/j.neucli.2017.03.001
Disclaimer – These blogs are for general information purposes only. Medical information changes daily, so information contained within these blogs may become outdated over time. In addition, please be aware that the information contained in these blogs is not intended as a substitute for medical advice or treatment and you should always consult a licensed health care professional for advice specific to your treatment or condition. Any reliance you place on this information is therefore strictly at your own risk.